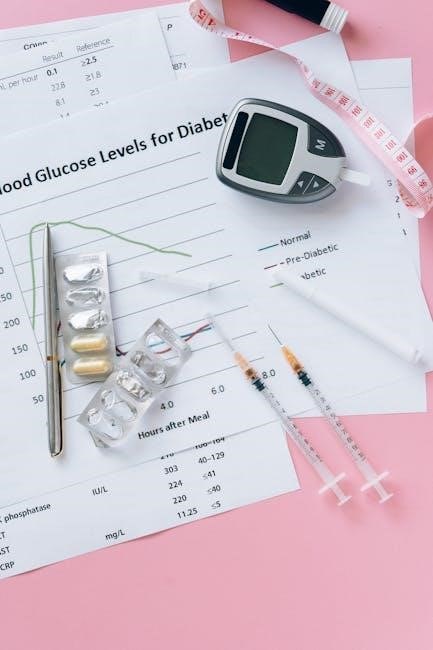
Understanding Sliding Scale Insulin Charts
Sliding scale insulin charts, often available as PDF resources, dictate insulin dosage based on current blood glucose levels, offering a flexible approach to diabetes management.
What is a Sliding Scale?
A sliding scale is a method used to determine insulin dosage, primarily in hospital settings and sometimes at home, based on a patient’s current blood glucose level. Unlike a fixed insulin regimen, the dosage adjusts “slides” up or down depending on the reading. These scales are frequently distributed as PDF charts for easy reference by healthcare professionals and patients.

The core principle involves correlating specific blood glucose ranges with corresponding insulin unit amounts. For example, a reading between 150-199 mg/dL might warrant 1 unit of regular insulin, while 200-249 mg/dL could require 2 units. These charts, often in PDF format, provide a quick guide for insulin administration.
The Purpose of Insulin Sliding Scales
The primary purpose of insulin sliding scales, often accessed as convenient PDF documents, is to provide a reactive, rather than proactive, approach to blood glucose control. They aim to correct hyperglycemia – high blood sugar – by administering insulin in response to elevated readings. These scales are particularly useful in situations where a patient’s insulin needs are fluctuating, such as during illness, stress, or changes in diet.
PDF versions of these charts offer a readily available guide for healthcare staff. However, it’s crucial to understand they aren’t a long-term solution. They address immediate glucose levels but don’t necessarily address underlying insulin resistance or inadequate basal insulin. The goal is temporary correction, documented in the dosage PDF.
Types of Insulin Used in Sliding Scales
Several insulin types are commonly utilized within sliding scale protocols, often detailed in accessible PDF dosage guides. Humulin R (regular insulin) is frequently employed due to its relatively rapid onset, allowing for quicker blood glucose correction. Humulin N (NPH insulin), an intermediate-acting insulin, may be used in some scales, though less common for immediate correction.
More modern sliding scale PDFs increasingly feature rapid-acting insulin analogs like Insulin Aspart (Novolog). These offer a faster and more precise response. The choice of insulin impacts the dosage and timing outlined in the chart. Understanding the pharmacokinetic profile of each insulin type is vital when interpreting a sliding scale PDF.
Humulin R (Regular Insulin)
Humulin R, a short-acting insulin, is a cornerstone of many sliding scale insulin charts, often found in downloadable PDF formats. Its use stems from its ability to rapidly lower blood glucose levels, making it suitable for correcting hyperglycemia as indicated by the chart’s dosage guidelines. These PDF resources detail specific unit adjustments based on pre-meal or bedtime glucose readings.
When utilizing Humulin R via a sliding scale, careful attention to the chart is crucial. The PDF will outline the corresponding insulin units to administer for various blood glucose ranges. It’s important to remember Humulin R’s peak action, as this influences the timing of subsequent glucose checks, as detailed within the chart’s instructions.
Humulin N (NPH Insulin)
Humulin N, an intermediate-acting insulin, appears less frequently as the primary correction insulin on sliding scale charts available as PDF documents, but may be included for basal coverage adjustments. PDF resources will illustrate how Humulin N is used to provide a background level of insulin, influencing the overall dosage strategy. Unlike rapid-acting insulins, its slower onset requires careful consideration when interpreting the chart.
While not typically used for immediate glucose correction, Humulin N’s dosage on a sliding scale PDF might be adjusted based on consistent glucose patterns. The chart will specify how to modify the nightly insulin amount, aiming for improved glycemic control. Understanding its prolonged action is vital when following the PDF’s guidance.
Insulin Aspart (Novolog)
Insulin Aspart (Novolog) frequently features prominently on sliding scale insulin charts, often distributed as PDFs, due to its rapid onset. These PDF resources detail specific dosage recommendations based on blood glucose ranges, providing a quick-acting correction. A typical chart will outline insulin units to administer for varying glucose levels, such as initiating hypoglycemia management below 60 mg/dL;
PDF versions of Novolog sliding scales often categorize glucose levels into narrow bands, prescribing precise insulin amounts. For example, a chart might indicate no coverage for levels under 149 mg/dL, escalating to 2 units or more for higher readings. Careful interpretation of these PDF charts is crucial for safe and effective dosage adjustments.
How Sliding Scale Charts Work
Sliding scale charts, often in PDF format, correlate blood glucose ranges with specific insulin unit dosages, guiding adjustments for optimal glycemic control.
Blood Glucose Ranges and Insulin Units
Sliding scale insulin charts, frequently accessed as PDF documents, categorize blood glucose levels into distinct ranges, each corresponding to a prescribed insulin unit dosage. For instance, a reading below 60 mg/dL typically initiates hypoglycemia management protocols, requiring no further insulin. Ranges between 60-149 mg/dL may also warrant no coverage.
As blood glucose rises, the insulin requirement increases incrementally. A level of 125-150 mg/dL might call for 2 units of regular insulin, while 151-200 mg/dL could necessitate 4 units. Medium-dose scales may offer no additional insulin for levels between 71-119 mg/dL. These PDF charts provide a structured framework for adjusting insulin based on individual needs and blood sugar fluctuations, ensuring a tailored approach to glycemic control.
Calculating Insulin Dosage
Calculating insulin dosage using a sliding scale chart, often found as a PDF, involves identifying the patient’s current blood glucose level and referencing the corresponding insulin unit recommendation. These charts typically operate on the principle of correcting hyperglycemia with small, incremental insulin doses.
For example, if a chart indicates 2 units for a blood sugar of 125-150 mg/dL, that’s the amount administered. Some scales aim for a BG drop of 50 mg/dL per insulin unit. It’s crucial to understand the specific scale’s parameters, as variations exist. Always verify the insulin type (Humulin R, Novolog, etc.) specified on the PDF and adhere to the prescribed administration guidelines;
Example Sliding Scale Charts
Numerous sliding scale charts are available as PDF documents, showcasing diverse approaches to insulin dosage. A Humalog sliding scale example might prescribe “No Coverage” for BG 60-124 mg/dL, then 2 units for 125-150 mg/dL, escalating with higher glucose levels.
A medium dose chart could differ: ≤70 mg/dL triggers hypoglycemia treatment, 71-119 mg/dL requires no additional insulin, while 120-150 mg/dL warrants 2 units, and 151-200 mg/dL, 4 units. These PDF examples demonstrate the variability; some scales are “resistant/high,” like Insulin Aspart scales. Always prioritize the chart provided by the patient’s healthcare team, ensuring it aligns with their individual needs and insulin type.
Humalog Sliding Scale Coverage Example
A typical Humalog sliding scale, often found as a PDF, illustrates insulin dosage adjustments based on blood glucose readings. For levels below 60 mg/dL, the protocol directs initiating hypoglycemia management and contacting a physician immediately. Between 60-149 mg/dL, no Humalog insulin is administered.
As blood glucose rises, the dosage increases. For example, a reading of 150-199 mg/dL might require 2 units of Humalog, while 200-249 mg/dL could necessitate 4 units. Higher ranges, exceeding 250 mg/dL, often call for 6 or more units, as determined by the physician’s orders detailed in the PDF chart. These charts are crucial for safe and effective insulin management.
Medium Dose Sliding Scale Example
A medium-dose sliding scale, commonly distributed as a PDF, provides a structured approach to insulin administration. If a patient’s blood glucose is less than or equal to 70 mg/dL, the protocol directs treatment for hypoglycemia following established nursing guidelines. For readings between 71-119 mg/dL, no additional insulin is indicated.
As glucose levels increase, insulin dosage is adjusted. A reading of 120-150 mg/dL typically warrants 2 units of insulin, while 151-200 mg/dL may require 4 units. These charts, available in PDF format, are essential tools for healthcare professionals, ensuring consistent and appropriate insulin delivery based on individual patient needs and physician orders.
Factors Affecting Insulin Dosage
Determining appropriate insulin dosage, even with a sliding scale chart (often found as a PDF), isn’t solely based on blood glucose. Basal insulin requirements – the long-acting insulin needed to maintain glucose control between meals and overnight – significantly impact correction doses. Patients needing higher basal rates may require adjusted sliding scale parameters.
Furthermore, individual patient needs vary greatly. Factors like diet, activity level, illness, and stress all influence glucose levels and, consequently, insulin sensitivity. A standardized PDF chart serves as a guide, but healthcare providers must personalize the scale, considering these variables to optimize glycemic control and prevent hypoglycemia or hyperglycemia.
Basal Insulin Requirements
Understanding a patient’s basal insulin needs is crucial when utilizing a sliding scale chart, often accessed as a PDF document. This refers to the long-acting insulin dose covering glucose management between meals and overnight. Inadequate basal rates can lead to consistently high or low blood sugars, rendering the sliding scale less effective.
Studies indicate patients with higher prandial (mealtime) insulin requirements often need nearly double the basal insulin. Therefore, a sliding scale, even a detailed PDF version, shouldn’t compensate for insufficient basal coverage. Healthcare professionals must first optimize basal rates before relying heavily on correction doses outlined in the chart for effective glucose control.
Individual Patient Needs

Sliding scale insulin charts, even those downloaded as a convenient PDF, are not “one-size-fits-all” solutions. Each patient exhibits unique responses to insulin, influenced by factors like weight, activity level, diet, and overall health. A chart providing a standardized dosage may require significant adjustments.

Therefore, healthcare providers must personalize the sliding scale based on individual sensitivity. Some patients might require smaller correction doses to achieve the same blood glucose reduction, while others need larger amounts. Regularly reviewing the patient’s response to the insulin, as guided by blood glucose monitoring, is vital for optimizing the PDF-based chart and ensuring safe, effective diabetes management.

Using a Sliding Scale Insulin Chart
Effective use of a sliding scale insulin chart, often accessed as a PDF, requires consistent blood glucose monitoring and precise insulin dosage administration.
Monitoring Blood Glucose Levels
Frequent blood glucose monitoring is paramount when utilizing a sliding scale insulin chart, often found as a downloadable PDF. Consistent checks – typically before meals, at bedtime, and when experiencing hypoglycemic symptoms – provide the data necessary for accurate insulin dosage adjustments.
The PDF chart translates these readings into specific insulin unit recommendations. Patients must understand their target blood glucose range and how to correctly operate their glucose meter. Accurate monitoring ensures the sliding scale effectively corrects hyperglycemia while minimizing the risk of hypoglycemia. Regular logging of results, alongside insulin doses, aids in identifying patterns and optimizing the sliding scale’s effectiveness, potentially requiring physician consultation for adjustments.
Administering Insulin Correctly
Proper insulin administration is crucial when following a sliding scale, often detailed in a PDF chart. Always verify the insulin type and concentration before drawing up the dose, referencing the chart for the correct units based on the current blood glucose level.
Utilize proper injection technique – rotating injection sites within a designated area to prevent lipohypertrophy. Subcutaneous injections are standard, but confirm with your healthcare provider. Double-check the insulin dosage with another person if possible, especially when using a sliding scale for the first time. Discard used needles safely and understand the storage requirements for your specific insulin type, as outlined in the PDF guide.
Hypoglycemia Management
When utilizing a sliding scale insulin chart (often found as a PDF), recognizing and promptly treating hypoglycemia is paramount. A chart will typically define blood glucose levels requiring intervention. If blood glucose drops below 60 mg/dL, immediate action is needed – consume 15-20 grams of fast-acting carbohydrates, like glucose tablets or juice.
Recheck blood glucose after 15 minutes; if still low, repeat carbohydrate intake. Severe hypoglycemia, causing confusion or loss of consciousness, requires glucagon administration or emergency medical assistance. Always have a readily available source of fast-acting glucose and inform family members about hypoglycemia symptoms and treatment, referencing the PDF’s guidance for specific thresholds and actions.
When to Contact a Physician
While a sliding scale insulin chart (available as a PDF) aids management, certain situations necessitate immediate physician contact. Consistently high or low blood glucose readings despite chart adherence warrant review of the insulin regimen. Any unexplained changes in insulin sensitivity or frequent hypoglycemic episodes require medical evaluation.
If you experience persistent symptoms despite following the sliding scale, or if you are unable to effectively manage your blood sugar levels using the provided PDF guidelines, consult your doctor. Additionally, report any new medical conditions, medications, or changes in diet, as these can impact insulin needs. Prompt communication ensures optimal diabetes control.

Sliding Scale Insulin Charts: PDF Resources
Numerous online sources offer downloadable sliding scale insulin chart PDF versions, providing convenient access to dosage guidelines for effective blood glucose control.
Finding Reliable PDF Charts Online
Locating trustworthy sliding scale insulin chart PDF resources requires careful consideration. Hospitals and reputable diabetes organizations frequently publish these charts for patient education and clinical use. Always prioritize sources affiliated with healthcare institutions or recognized medical societies to ensure accuracy and safety.
A quick internet search reveals numerous options, but verifying the chart’s origin is crucial. Look for charts displaying clear dosage instructions correlated with specific blood glucose ranges. Ensure the chart specifies the type of insulin (Humulin R, Novolog, etc.) it applies to, as dosage varies significantly. Be wary of charts lacking a clear source or appearing outdated. Cross-reference information with your healthcare provider to confirm the chart aligns with your individual treatment plan. Downloading PDFs directly from hospital websites or professional medical groups is generally the safest approach.
Understanding Chart Variations
Sliding scale insulin chart PDF documents aren’t standardized; significant variations exist depending on the hospital, physician preference, and individual patient needs. Some charts utilize a “less than/equal to” format for blood glucose ranges, while others employ specific numerical boundaries. Dosage increments also differ – some charts increase insulin by 1 unit, while others use 2 or even 4-unit steps.
Furthermore, the insulin type dictates the chart’s structure. A Humalog sliding scale will differ from a Humulin R chart due to differing onset and duration of action. “Medium dose” charts, for example, may start coverage at higher blood glucose levels than standard scales. Always confirm the chart’s intended insulin and range applicability. Understanding these nuances is vital; never assume one chart fits all situations. Always consult your healthcare provider for clarification.
Limitations and Considerations
Sliding scale insulin chart PDF use carries risks, potentially leading to inconsistent dosage and reactive hyperglycemia; alternatives like basal-bolus regimens are often preferred.
Potential Risks of Sliding Scales
Employing a sliding scale insulin chart, even in PDF format, isn’t without potential drawbacks. A primary concern is reactive hyperglycemia – where blood glucose levels repeatedly spike and fall, demanding increasingly larger insulin dosages. This cycle doesn’t address underlying insulin resistance or inadequate basal rates;
Furthermore, relying solely on correction doses can delay appropriate adjustments to long-acting insulin. The frequent dosage changes inherent in sliding scales increase the risk of medication errors and hypoglycemia, particularly in vulnerable populations. Patients may experience significant variability in blood sugar control, hindering effective diabetes management.
The reactive nature of sliding scales doesn’t proactively address the root causes of hyperglycemia, potentially masking the need for comprehensive treatment plan revisions. Careful monitoring and physician oversight are crucial when utilizing this approach.
Alternatives to Sliding Scales
Moving beyond a simple sliding scale insulin chart (often found as a PDF), more effective diabetes management strategies exist. Prioritizing basal insulin optimization – adjusting long-acting insulin to meet individual needs – provides a stable glucose baseline, reducing reliance on correction doses.
Carbohydrate counting, coupled with bolus insulin dosage adjustments, offers greater precision. Continuous Glucose Monitoring (CGM) provides real-time data, enabling proactive adjustments and minimizing fluctuations. Comprehensive diabetes education empowers patients to self-manage effectively.
Insulin pump therapy delivers a customizable basal rate and bolus doses, offering flexibility and improved control. Regularly reviewing and adjusting the entire insulin regimen, rather than solely reacting to high blood sugar, is paramount. These alternatives promote sustainable glucose management and reduce risks associated with reactive approaches.
